Covid-19, Employers, Health Benefits and a Safe Workplace
While many US companies are considering returning to work in an office, they are weighing on the decisions to make on Covid-19.
CMS issued guidance on August 19th, removing barriers to COVID-19 diagnostic testing and vaccinations and strengthening requirements that plans and issuers cover diagnostic testing and vaccines administration without cost-sharing, prior authorization, or other medical management requirements imposed by the plan or issuer. For example, covered individuals wanting to ensure they are COVID-19 negative prior to visiting a family member would be able to be tested without paying a copay.
The vaccine itself will be paid for through funding authorized by the Coronavirus Aid, Relief, and Economic Security (CARES) Act, but administration of the vaccine by a provider will be paid for by the plan sponsor (employer or insurer).
Issuers of a non-grandfathered group or individual health insurance coverage are required to cover without cost-sharing the vaccine and its administration when provided by a network provider, and during the COVID-19 PHE (Public Health Emergency), are also required to cover without cost-sharing the vaccine and its administration when provided by an out-of-network provider. Providers are prohibited by agreement with the U.S. Government from billing patients for the vaccine or its administration, including balance billing.
Vaccine mandates
You probably read about the 200$ penalty an airline company imposed to non-vaccinated employees. You should know that many employers are considering it, especially since the FDA’s Pfizer vaccine approval. Following a recent survey by Mercer, a solid majority of 66% of the surveyed employees said they would want their own employer to implement a vaccine mandate; only 21% opposed.
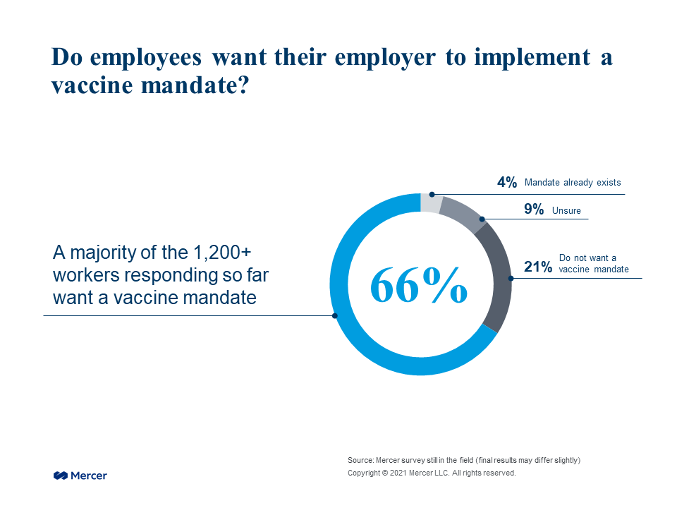
The percentage of employees who want their employers to implement a vaccine mandate seems roughly equivalent to the percentage of Americans of working age who are vaccinated, the author noticed.
This has some employers turning to alternative strategies to encourage vaccination, such as a premium surcharge on health insurance (like Delta Airlines did, with a hefty 200$ monthly surcharge…).
Other alternatives to vaccination include stricter masking protocols and regular testing for the virus, as well as restrictions on travel and client meetings. If feasible, employers can give the non-vaccinated the opportunity to continue to work remotely (they just need to be careful that they don’t give only the non-vaccinated work flexibility).
One way or another, employers will need to demonstrate that they have a safe workplace.
We would be interested to know what employers in the FACC-NY network are considering doing on these issues in the coming months.
We can send anyone who is interested, the 18-page resource from the CDC providing extensive information on what health plans have to cover with regard to COVID-19 expenses, you can also download it here: https://www.cms.gov/covidvax
This #MemberInsights article is authored by Care2Care International.